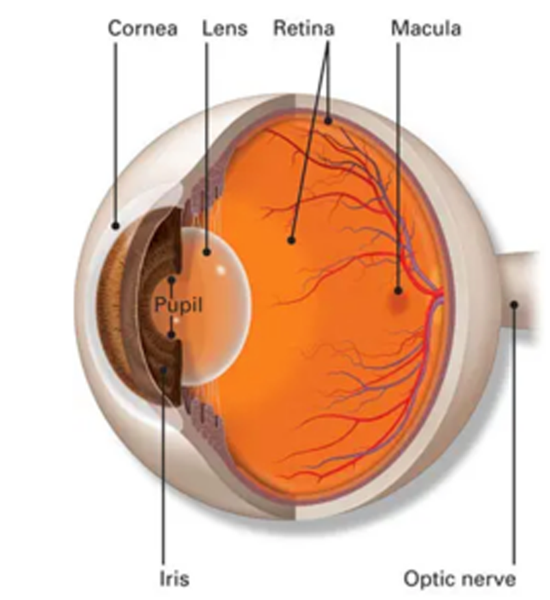
Retina
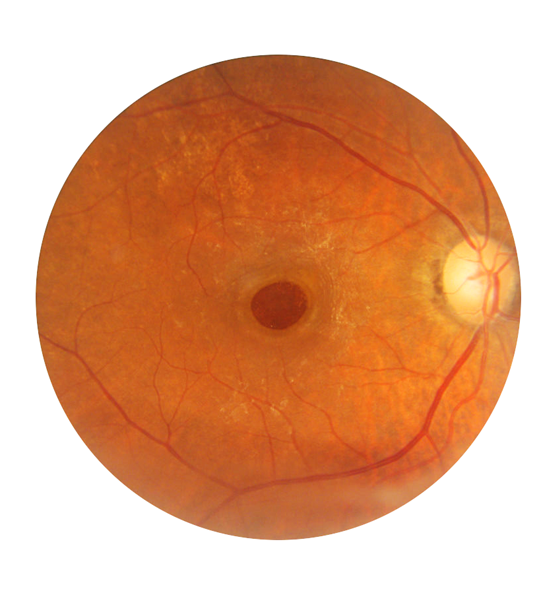
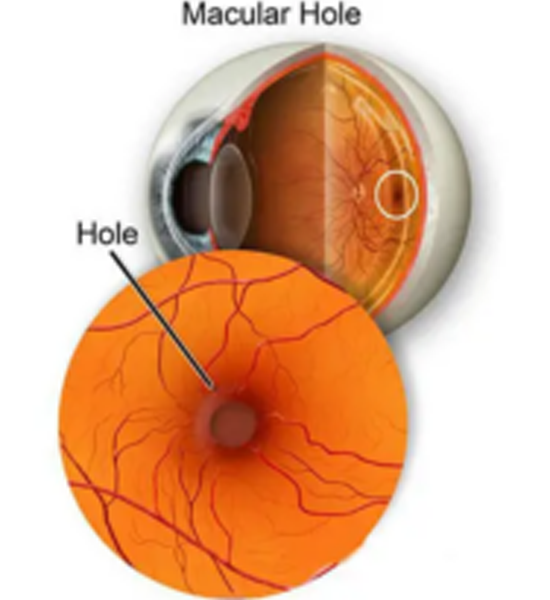
Macular hole is when a circular opening forms in your macula. As the hole forms, things in your central vision will look blurry, wavy or distorted. As the hole grows, a dark or blind spot appears in your central vision. A macular hole does not affect your peripheral (side) vision.
What causes
a Macular hole?
Age is the most common cause of macular hole. As you get older, the vitreous begins to shrink and pull away from the retina. Usually the vitreous pulls away with no problems. But sometimes the vitreous can stick to the retina. This causes the macula to stretch and a hole to form.
Sometimes a macular hole can form when the macula swells from other eye disease. Or it can be caused by an eye injury.
How will my eye doctor check for
a macular hole?
Your eye doctor will check for a macular hole by doing a test called an optical coherence tomography (OCT). This is a painless test that uses light waves to take detailed pictures of your retina.
Before the test, we may give you some eye drops to dilate (widen) your pupil.
What’s the treatment
for a macular hole?
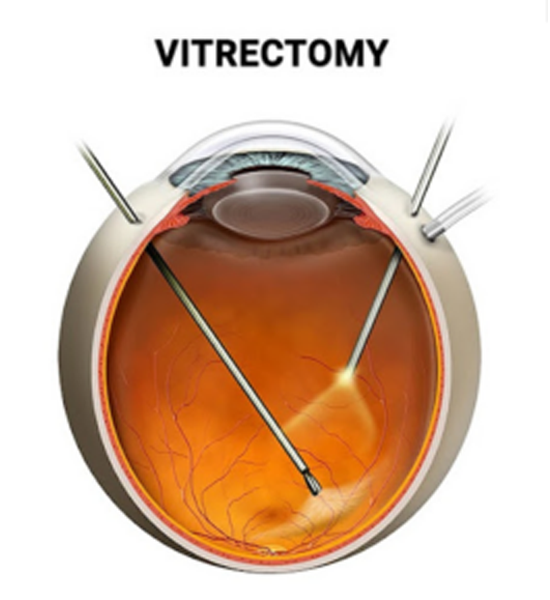
If a macular hole is affecting your vision, you’ll probably need a type of surgery called vitrectomy to fix the hole and prevent permanent vision loss.
During a vitrectomy,we will remove the vitreous and some tissues on the surface of the macula and injects a gas bubble into your eye. The bubble is like a temporary bandage that holds the edges of the macular hole together and helps your eye close the hole.
After the surgery, you’ll need to limit your activities and movement for a while.
You also need to avoid flying or getting nitrous oxide (laughing gas) for any procedures until the bubble is completely gone — these things can affect the pressure in your eye.
Treatment works best when we catch macular holes early, so it’s important to talk to us right away if you notice any unusual symptoms.
ERM
(epi-retinal membrane)
ERMs can be diagnosed during a routine vision exam. In many cases, vision is not affected. Most types of ERM do not change and cause vision symptoms.
Some ERM do get worse, however, and will cause blurring and vision disturbances. The only time we will suggest treatment is when there are vision symptoms.
A diagnostic test called optical coherence tomography (OCT) which uses light waves to scan and view the layers of the retina, can help with the diagnosis of ERMs.
We may also use another test called fluorescein angiography. This test involves the use of dye to light up areas of the retina.
Vitrectomy surgery
procedure
The surgery for ERMs is called a vitrectomy. During a vitrectomy, we will make tiny cuts in the affected eye and remove the fluid from inside the eye.
What are the symptoms of
retinal detachment?
Your eye doctor will check for a macular hole by doing a test called an optical coherence tomography (OCT). This is a painless test that uses light waves to take detailed pictures of your retina.
Before the test, we may give you some eye drops to dilate (widen) your pupil.
What are the symptoms of
retinal detachment?
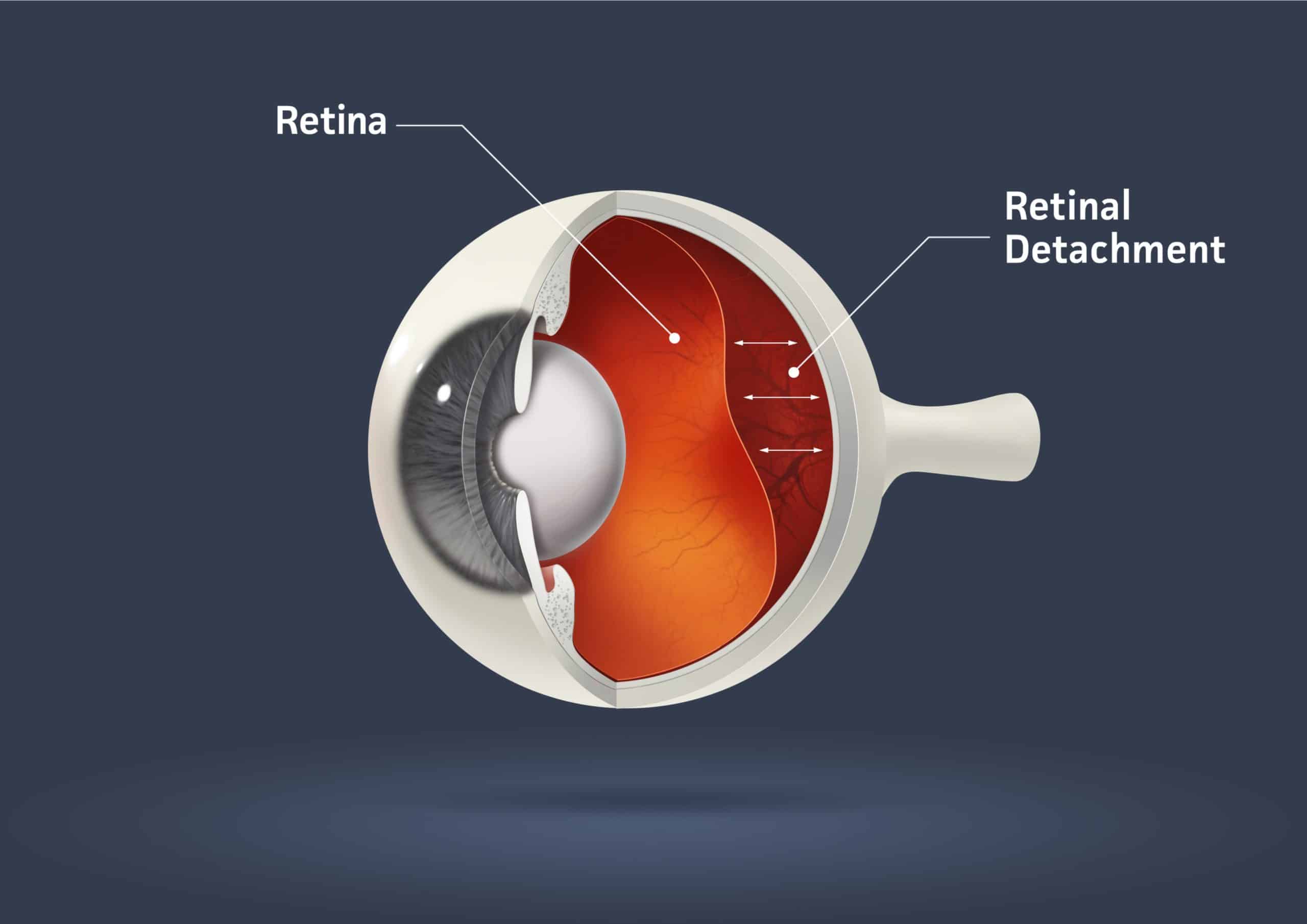
If only a small part of your retina has detached, you may not have any symptoms.
But if more of your retina is detached, you may not be able to see as clearly as normal, and you may notice other sudden symptoms, including:
- A lot of new floaters (small dark spots or squiggly lines that float across your vision)
- Flashes of light in one eye or both eyes
- A dark shadow or “curtain” on the sides or in the middle of your field of vision
Retinal detachment
is a medical emergency
If you have symptoms of a detached retina, it’s important to go to your eye doctor or the emergency room right away.
The symptoms of retinal detachment often come on quickly. If the retinal detachment isn’t treated right away, more of the retina can detach — which increases the risk of permanent vision loss or blindness.
How can I prevent
retinal detachment?
Since retinal detachment is often caused by aging, there’s often no way to prevent it. But you can lower your risk of retinal detachment from an eye injury by wearing safety goggles or other protective eye gear when doing risky activities, like playing sports.
If you experience any symptoms of retinal detachment, go to your eye doctor or the emergency room right away. Early treatment can help prevent permanent vision loss.
It’s also important to get comprehensive dilated eye exams regularly. A dilated eye exam can help your eye doctor find a small retinal tear or detachment early, before it starts to affect your vision.
Am I at risk for retinal detachment?
Anyone can have a retinal detachment, but some people are at higher risk. You are at higher risk if:
- You or a family member has had a retinal detachment before
- You’ve had a serious eye injury
- You’ve had eye surgery, like surgery to treat cataracts
Some other problems with your eyes may also put you at higher risk, including:
- Diabetic retinopathy (a condition in people with diabetes that affects blood vessels in the retina)
- Extreme nearsightedness (myopia), especially a severe type called degenerative myopia
- Posterior vitreous detachment (when the gel-like fluid in the center of the eye pulls away from the retina)
- Certain other eye diseases, including retinoschisis (when the retina separates into 2 layers) or lattice degeneration (thinning of the retina).
How can I prevent retinal detachment?
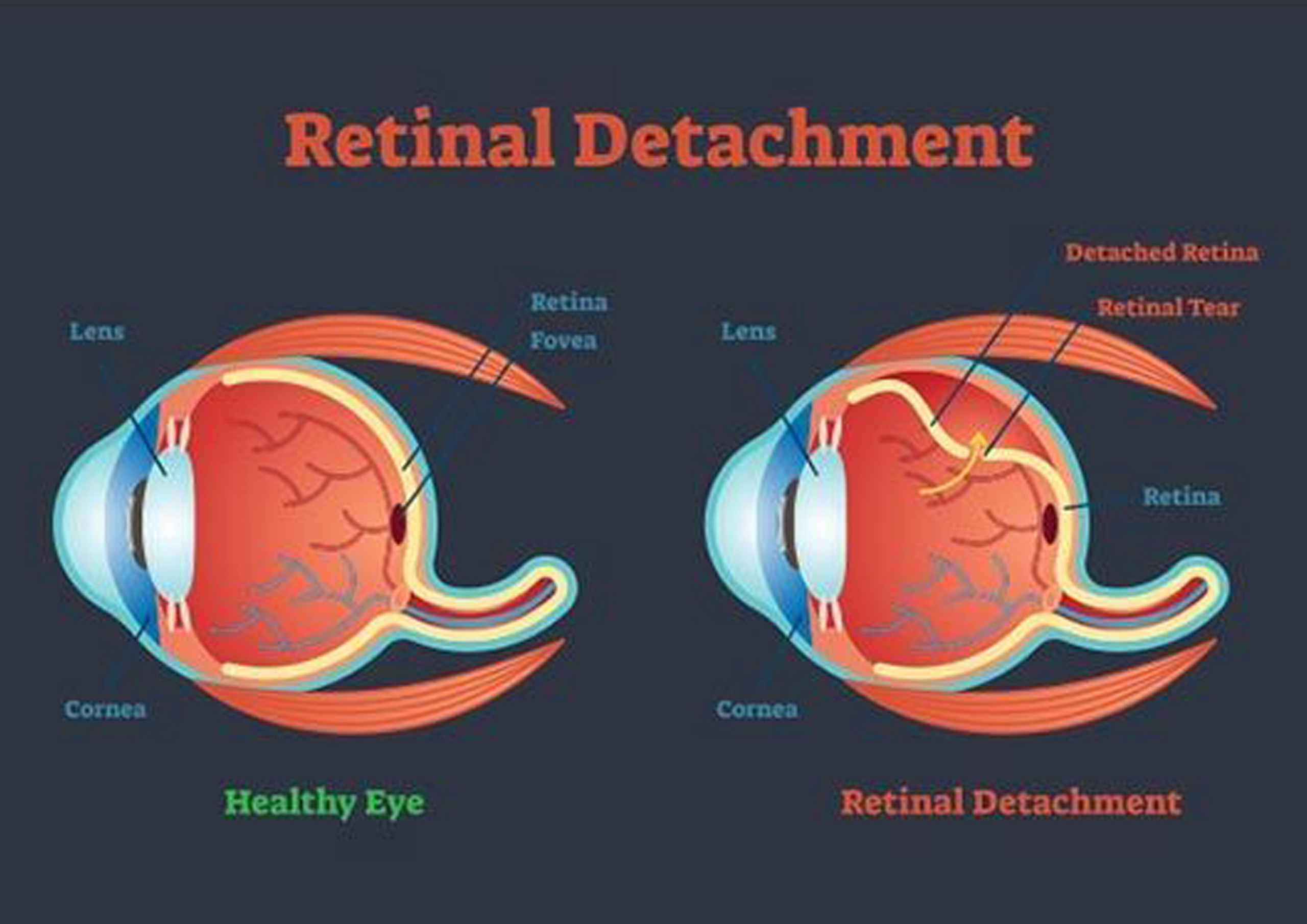
There are many causes of retinal detachment, but the most common causes are aging or an eye injury.There are 3 types of retinal detachment:
Rhegmatogenous, Tractional, Exudative.
Each type happens because of a different problem that causes your retina to move away from the back of your eye.