keratoconus
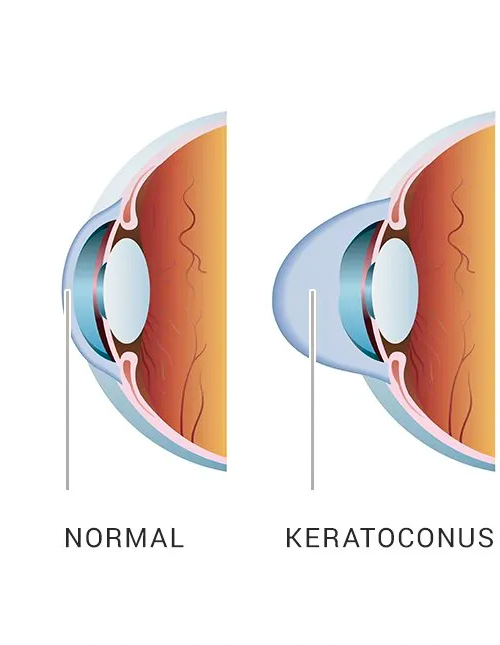
WHAT IS KERATOCONUS? Keratoconus usually appears in individuals during their late teens or early twenties and usually progresses for 10-20 years as the cornea steepens and thins. Keratoconus almost always affects both eyes, but usually, one eye will advance sooner than the other. Studies show that while keratoconus affected 1 out of every 2,000 people in the past, it now affects 1 in 400.
Symptoms of
Keratoconus
- Glare and halos around lights
- Blurring and distortion of vision
- Light sensitivity and irritation
- Difficulty seeing at nighttime
- Sudden worsening or clouding of vision
- Headaches that are associated with eye pain
- Corneal thinning, bulging, or rounding
Frequent changing of glasses or contact lens prescriptions, with high levels of astigmatism


Symptoms of
Keratoconus
- Glare and halos around lights
- Blurring and distortion of vision
- Light sensitivity and irritation
- Difficulty seeing at nighttime
- Sudden worsening or clouding of vision
- Headaches that are associated with eye pain
- Corneal thinning, bulging, or rounding
Frequent changing of glasses or contact lens prescriptions, with high levels of astigmatism
How is the cross-linking
procedure done?
The simple procedure is done in-the clinic and it is entirely painless.
1. A well trained technician will drop a special solution of riboflavin (B-vitamin) on your cornea for 30 minutes.
2. Next, your eyes will be exposed to 10-30 minutes of UV light. The intensity of these light waves are similar to the sterilizing blue lights you’ve seen at the deli counter.
Are there risks or complications
involved with CXL?
Epithelium off, which means the thin layer covering the eye’s surface is removed, allowing for faster penetration with liquid riboflavin, and more effective crosslinking. This is the type we perform, and are the best at getting the epithelium to grow back quickly without pain or scarring, because we perform nearly 1,000 PRK per year, where we also remove the epithelium and need it to grown back rapidly, so have THE experience.
Transepithelial corneal crosslinking (epithelium on) is where the corneal epithelial surface is left intact, which requires a longer riboflavin loading time. Many published studies have shown this method to be less effective than epi-off, and NO study has shown epi-on to be MORE effective–leading to the conclusion that epi-on is LESS effective than epi-off. So why leave the epithelium on, and have your CXL maybe not work–rather than get epi-off and have it be EFFECTIVE at a center that is EXPERIENCED at getting your epithelium to grow back quickly?
ARE THERE RISKS OR COMPLICATIONS
INVOLVED WITH CXL?
CXL as a treatment for keratoconus is a promising procedure that leads to very positive results – with minimal risks involved. It was approved for use in Europe over 10 years ago, and it has been performed safely and successfully on tens of thousands of patients worldwide.
Regarding complications, the most common complaint is that CXL doesn’t stabilize the cornea and the patient’s condition continues to deteriorate. Simply put, CXL doesn’t work. However, this is the same outcome as if the procedure was never done – so it isn’t much of a “complication.”
Very rarely, people experience scarring or haze as a complication, or they have endothelial decompensation that requires a corneal transplant to correct it. Of course, had many of these same patients not undergone CXL, they may have eventually needed a corneal transplant to treat their keratoconus.



BEST CANDIDATES
FOR CORNEAL
CROSSLINKING
- Patients with Corneal Ectactic Disorders (Keratoconus or Pellucid Marginal Degeneration)
- Patients with ectasia/regression/need a reoperation after LASIK
- Patients with high prescriptions or thin corneas considering cutting vision correction procedures such as LASIK might eventually be pre-treated with corneal crosslinking to strengthen the eye’s surface beforehand (this is known as the “Athens Protocol” and was developed by John Kannelopoulos, MD, who trained at Harvard with Dr. Chynn who trained Dr Omar
- PMD(Pellucid Marginal Degeneration)
What Can You Expect After Corneal
Crosslinking (CXL)?
- Improved Visual Acuity
- Decreased visual fluctuations
- Prevent need for corneal transplant after complicated/defective LASIK
What Should I Do if I’m Interested in CXL or Think
I Might Need It?
- Call or email our office to set up a CXL Consultation
Cross linking
+ PRK
In some cases of keratoconus (stage 1 and 2),and when your cornea is thick enough,in addition to the crosslinking,a PRK will be performed using the excimer laser before the crosslinking(at the same day) to remove your prescription (or the majority of it ).Dr omar has mastered this technique during his New York refractive surgery fellowship.

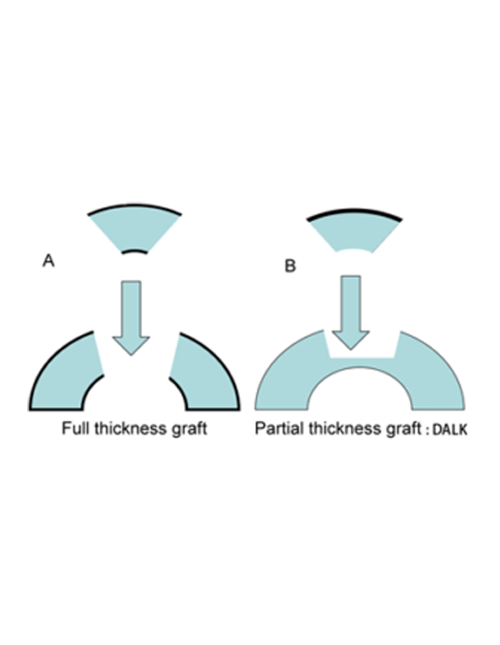
DALK
When the keratoconus is in a very advanced stage, a replacement of the cornea is indicated.Since the disease touches only the anterior 2 ⁄ 3 of the cornea ,it becomes obvious that there is no need to replace the posterior 1 ⁄ 3,that’s what Deep anterior Lamellar Keratoplasty is about !DALK is a modern technique whereby the outer two layers of the cornea are removed and replaced with the outer two layers from a donor cornea to give a partial-thickness transplant.
Advantage :
- Closed eye surgery
- No chance of blinding Endothelial rejection (by retaining the recipient’s own endothelial layer)
- Can always perform a Penetrating Keratoplasty if visual results are not satisfactory
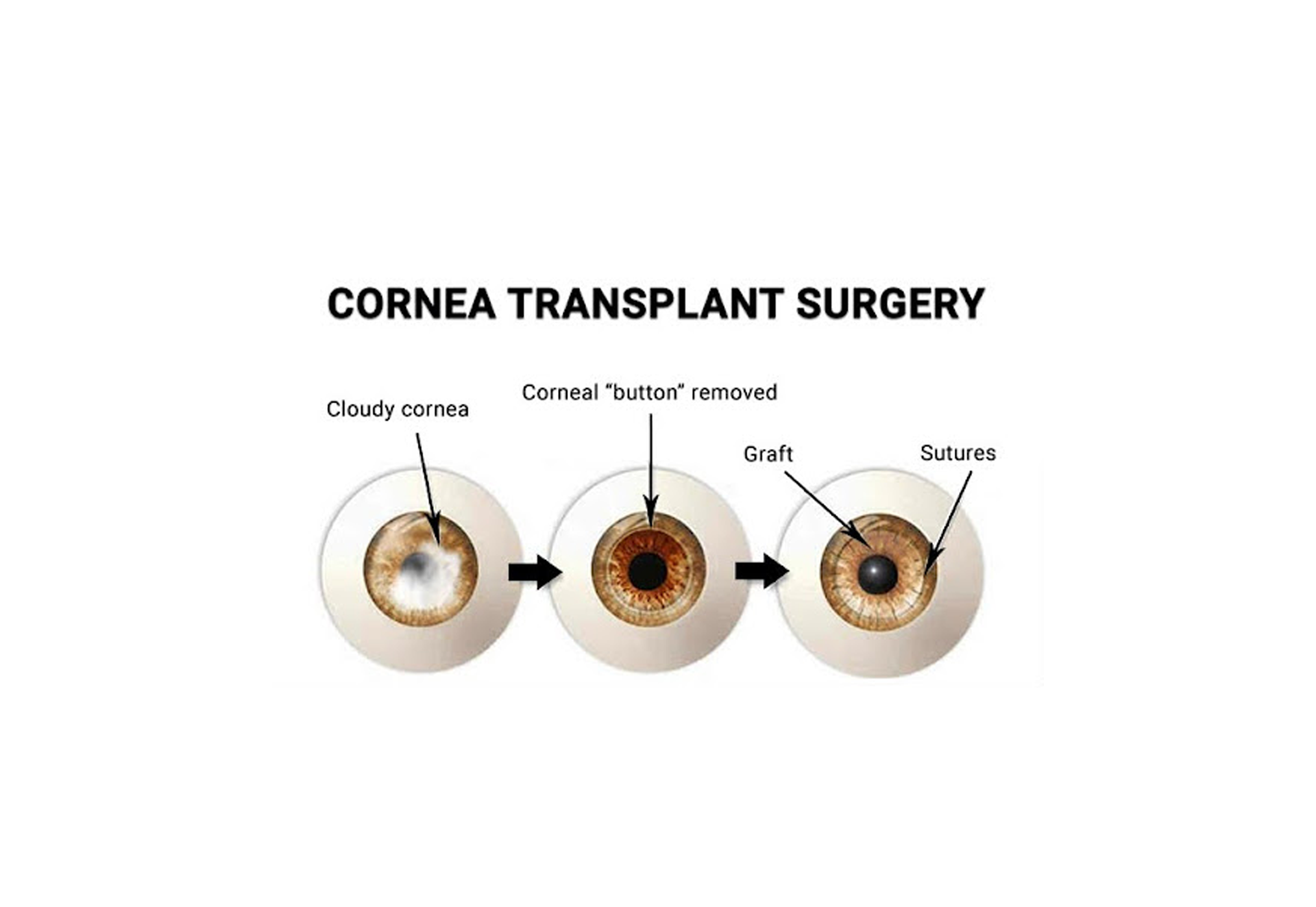
Penetrating
keratoplasty
Historically, penetrating keratoplasty (PK) has been the gold standard surgical approach for the treatment of advanced keratoconus. In contemporary practice, however, deep anterior lamellar keratoplasty (DALK) is increasingly becoming the preferred primary surgical option. PK, nonetheless, has a significant role in the surgical management of keratoconus, especially where there is deep stromal scarring, a history of corneal hydrops, or, less commonly, coexisting endothelial dysfunction.